Doctors gang up against clinical officers on C-section surgeries row

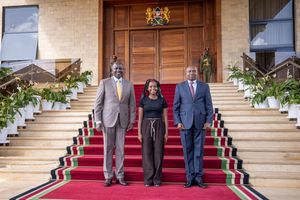
Kenya Union of Clinical Officers national chairman Peterson Wachira (centre) and other officials address journalists outside the union’s offices yesterday. They called on the government to offer the staff contracted under the Universal Health Care programme permanent jobs and to immediately post all interns.
What you need to know:
- The associations added: “The independent performance of such procedures by cadres without the requisite surgical training, accreditation, and oversight, directly endangers the lives of mothers and newborns. Maternal mortality and morbidity remain a national concern, and inappropriate delegation of surgical responsibilities risks worsening this crisis further.”
Doctors, obstetricians, and gynaecologists have ganged up against clinical officers over the multi-million-shillings caesarian section operations, saying the latter have no “requisite surgical training, accreditation, and oversight.”
Under the Kenya Medical Association (KMA), and the Kenya Obstetrical and Gynaecological Society (KOGS), the medics say such surgical operations like the caesarian section should not be practiced independently by clinical officers.
“Surgery, particularly obstetric and gynaecologic surgery, requires highly specialised training, rigorous and continuous competency assessments, and strict adherence to globally accepted medical and surgical safety standards,” read the statement in part.
The associations added: “The independent performance of such procedures by cadres without the requisite surgical training, accreditation, and oversight, directly endangers the lives of mothers and newborns. Maternal mortality and morbidity remain a national concern, and inappropriate delegation of surgical responsibilities risks worsening this crisis further.”
The associations further went ahead to call upon the Ministry of Health, relevant stakeholders, and Parliament to “invest in training more medical specialists and medical officers to meet the growing demand for surgical services while ensuring patient safety is not compromised.”
They also urged the ministry and Parliament to ensure that modifications to healthcare practices are “backed by scientific evidence and rigorous competency-based training rather than political negotiations”, and to “maintain a structured team-based approach where all professionals work within their regulated scope of practice to enhance patient outcomes rather than compromise them.”
“Surgical procedures should be conducted by professions legally recognised and adequately trained to perform them including the facilitation of medical training via formal medical schools for clinical officers who wish to pursue this path,” the two associations said.
This is despite a circular issued in 2008 by the then Director of Medical Services, Dr Francis Kimani, to all eight provinces at the time, affirming that clinical officers in reproductive health were well-trained and could perform cesarean sections and other surgical procedures.
The circular read: “The Ministry of Health has recognised the skills and competencies of clinical officers in reproductive health. Their training started at Kenya Medical Training College in the year 2002 to address various obstetric emergencies especially where there is no obstetrician or gynaecologist. This will go a long way in reducing maternal mortality and improving maternal health.”
It further noted: “Under the transfer of skill policy, clinical officers in reproductive health can perform the following procedures: cesarean section, bilateral tubal ligations, dilatation and curettage, Manual Vacuum Aspiration, Macdonald stitch insertion, running of high-risk clinics, conducting ward rounds and any other reproductive health duties assigned to them by the obstetrician or gynaecologist.”
Now, Peterson Wachira, the chairperson of the Kenya Union of Clinical Officers (KUCO), says that the fight, which has only started after 17 years of silence, has nothing to do with safety and quality of service, but rather “market and monetary considerations.”
“Degree Clinical officers are taught anatomy for two years which includes cadavership, hence giving them similar knowledge of anatomy to medical officers. In Tanzania, Ghana, and Malawi, clinical officers perform the Caesarian section at the diploma level, and in Zambia at the degree level. Researches done in different countries have shown no difference in outcomes of cesarean section outcomes between clinical officers and medical officers,” said Mr Wachira.
Data from the Kenya National Bureau of Statistics show that births through C-sections have almost doubled, from nine per cent in 2014 to 17 per cent in 2022.
Of the 1.24 million hospital deliveries that Kenya had in 2022, 211,227 were through C-sections compared with 110,909 in 2014 when the total deliveries in hospitals were 895,400.
Hospitals such as M.P Shah, Aga Khan Hospital, Nairobi Hospital, and Mater Hospital, in 2022, were charging at least Sh210,000 for C-sections, with emergency C-sections hitting above Sh300,000.
Normal deliveries ranged between Sh80,000 and Sh100,000 in the same hospitals. The costs have been rising in line with inflation.
The Global Association of Clinical Officers and Physician Associates (GACOPA) also denounced the statement, terming it as “malicious, misleading and outright deceptive”, and accused KMA, KOGS, and the World Medical Association, who issued a supporting statement, of “trying to maintain a monopoly over healthcare at the cost of human lives.”
The global association asserts that clinical officers have been performing life saving surgeries, including C-sections, hernia repairs, and orthopaedic procedures, for decades, with outcomes matching or surpassing those of doctors, especially in hospitals where doctors are absent. They refute claims that clinical officers are unqualified, emphasising their rigorous medical and surgical training, internships, and licensing.
Citing studies from BMJ, The Lancet, and WHO, GACOPA dismisses concerns over patient safety, arguing that restricting clinical officers only limits access to care.
They accuse WMA of gatekeeping healthcare instead of addressing doctor shortages and demand the withdrawal of misleading statements.