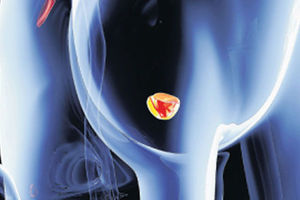
Treatment for testicular cancer usually starts with an orchiectomy, which involves surgically removing the affected testicle.
When it comes to men’s health, topics such as testicular cancer are not commonly discussed. Although rare, it is the most common cancer in young men aged 15 to 35 —a group who often feel invulnerable to serious illness.
In Kenya, the disease is still considered rare, with around 200 new cases reported each year, according to the World Health Organisation (WHO), often resulting in late diagnosis due to stigma, lack of awareness, and limited access to specialised care.
Samuel Ogombe, a consultant urologist and surgeon at AAR Hospital, says that in a clinic, he can never miss someone with a testicular issue. “Whether it’s cancer or not that is now variable, but you’ll definitely see someone with testicular cancer in a month, you may pick one or two,” he says.
The tragedy lies not only in the diagnosis, but also in the silence surrounding it.
Many young men ignore warning signs, delay seeking medical care, or are too embarrassed to talk about changes to their male reproductive organs.
As a result, a condition that could be quickly and effectively treated often progresses to an advanced stage because it remains unnoticed or unspoken of.
Doctors say that testicular cancer is one of the most treatable forms of cancer. According to global cancer data, the five-year survival rate exceeds 95 percent when the cancer is detected early.
Even in later stages, treatment can still be effective, although it becomes more intensive and carries greater risks.
Dr Ogombe notes that the earliest warning signs are often difficult to detect.
“The primary thing men should look for is swelling or a nodule in the testes. This is the most common presenting feature. The swelling is usually painless, which leads many to delay seeking help. It can grow quite large before someone decides to seek treatment,” says Dr Ogombe.
He says that other early signs may include a dull ache or a feeling of heaviness in the abdomen or scrotum. Less commonly, breast enlargement (gynaecomastia) may occur in men with certain germ cell tumours.
“Advanced disease, however, may present with more serious symptoms, such as back pain, chest discomfort, a persistent cough, bone pain, or even fractures if the cancer has spread,” he says.
Why men stay silent
Despite the high survival rate and the fact that screenings are easy to perform, Dr Ogombe notes that several cultural and psychological factors contribute to men remaining silent about changes to their testicles.
“Genitalia is an area that people struggle to discuss,” he explains. “By the time a patient seeks help, they’ve often suffered in silence and consulted friends. It’s just not part of our culture to speak openly about these issues.”
He notes that there are also myths surrounding masculinity. Some men fear that acknowledging a problem signifies weakness, while others dread the possibility of losing a testicle and how this might affect their sense of manhood.
Similarly, awareness levels about testicular cancer are low. Unlike breast cancer, which has benefited from campaigns promoting self-examination, testicular cancer lacks visibility, and many men are unaware that they should conduct self-examinations.
Risk factors and myths
Dr Ogombe states that the main risk factors include undescended testicles (cryptorchidism).
“If your testes are not in the correct position that is one of the major risk factors.”
Additional risk factors include family history (having a first-degree relative who has had testicular cancer increases the risk), previous history, and exposure to certain chemicals or drugs.
“Smoking is also considered a contributing risk factor,” he adds.
Contrary to popular belief, testicular cancer is not caused by trauma, diet, or sexual activity. Another common misconception is that it only affects older men. In reality, Dr Ogombe says that the peak age group for testicular cancer is 20 to 35 years old.
How to check for lumps in testes
"Be aware of your health. Examine yourself regularly. If you feel a lump, come to us early. Don’t wait until the tumors have spread to the lungs or liver, because treatment becomes much more difficult by then,” he explains.
Unlike women, who have structured guidelines for breast self-examinations, men are less consistent. Dr Ogombe recommends performing a self-exam once a month after a warm shower. Gently roll each testicle between your fingers to check for lumps, swelling, or changes in size. If you notice anything unusual, seek medical attention promptly.
While most swellings in the scrotum are not cancerous, only a doctor can confirm this. Failing to investigate a potentially harmful condition due to assuming it is harmless can have serious consequences.
So, what happens if the doctor confirms that the swelling is cancerous?
Treatment journey
Treatment for testicular cancer usually starts with an orchiectomy, which involves surgically removing the affected testicle. While this procedure may distress most men, it can be curative if performed early.
“It is a necessary step. Most men are concerned about the void left by the removal, but prosthetic testicles can be implanted. Importantly, many men continue to be fertile with just one testicle. You can live with one kidney or one testicle and still father children,” explains Dr Ogombe.
Patients may require chemotherapy or radiotherapy, which can affect fertility. Doctors often recommend sperm banking before treatment begins, in order to preserve fertility options.
Dr Ogombe emphasises that the survival rate for testicular cancer is almost 100 percent if it is detected early. Even in advanced cases, multimodal treatment can be effective, although it usually takes a heavier physical and emotional toll.
Can I get children?
Dr Ogombe says that one of the main concerns men have is whether testicular cancer will affect their ability to father children or have a normal sex life.
He reassures patients that most men with one healthy testicle produce enough testosterone and sperm to support fertility and sexual function.
“Typically, erections, sex drive, and the ability to father children are preserved,” he says.
However, chemotherapy and radiotherapy can reduce sperm count. For men who wish to have children in the future, sperm banking before treatment is highly recommended.
Beyond the physical effects, the psychological impact can also be significant. Some men may struggle with body image issues, anxiety about their masculinity, or depression following surgery. Support groups, counselling, and open conversations with partners and healthcare providers are crucial for recovery.
Follow-up care is essential, even after treatment. Patients require regular check-ups and blood tests to monitor tumour markers such as alpha-fetoprotein (AFP), beta-human chorionic gonadotropin (beta-HCG), and lactate dehydrogenase (LDH), as well as imaging tests to check for recurrence. Most relapses occur within the first two years, so ongoing surveillance is vital.