The Social Health Authority building in Nairobi.
A severe healthcare crisis is unfolding as thousands of patients seeking medical services in private hospitals are being turned away or forced to pay cash upfront.
This is after private facilities began rejecting the Social Health Authority (SHA) insurance cards, citing unpaid government debts.
At the centre of the crisis is the blacklisting of the SHA by private healthcare facilities under the Rural-Urban Private Hospitals Association (RUPHA) and the Kenya Association of Private Hospitals. The hospitals accuse the government of failing to pay billions of shillings owed for services rendered.
The situation is further compounded by outstanding liabilities from the defunct National Health Insurance Fund (NHIF), with hospitals demanding immediate settlement before resuming services under the SHA scheme.
This unprecedented standoff between healthcare providers and the Ministry of Health has left vulnerable patients stranded, with many unable to access critical care for serious conditions.
At the reception area of a well-known private hospital in Nairobi, Jane Mwikali, a 32-year-old mother, sits nervously clutching her son’s medical file. The child, battling a high fever and breathing difficulties, was referred here after a local clinic could not manage his condition.

Diana Akoth speaks during an interview at a bus stop outside Kenyatta National Hospital in Nairobi after a failed attempt to seek medical services on January 16, 2025.
“They told me my son won’t be seen unless I pay cash. I relied on my SHA cover. I have no money. Where do I go?” she asks, tears welling up in her eyes.
In Nyandarua, it was a double tragedy for Lydia Kuria, a patient from Ndaragua Constituency, whose Social Health Authority (SHA) card is linked to a private hospital that has suspended services due to unpaid government claims.
Despite her active subscription, she found herself unable to transfer her coverage to a public facility.
She told Nation she underwent surgery at the private hospital two weeks ago but, frustrated by repeated denial of medication, sought to shift her SHA subscription to Nyahururu Referral Hospital.
“I wanted to move to a public hospital because private facilities keep refusing to offer treatment due to non-payment by the government. Last Friday, knowing I had a follow-up clinic on Tuesday, I made one last attempt to transfer my SHA card to Nyahururu Hospital. But at the SHA offices, I was told transfers are not allowed. I don’t understand why it was automatic with NHIF,” she said.

Nyahururu County Referral Hospital.
By yesterday afternoon, she was still struggling to raise Sh3,000 for consultation fees and Sh4,000 for medication.
“The hospital insists I must pay in cash. They are not accepting the SHA card, yet I have contributed for over three months, as required before benefiting from the surgery I underwent,” she lamented.
The boycott by private hospitals has pushed more patients to public facilities like Nyahururu Referral Hospital.
In Maralal, Samburu County, several patients were left stranded after private hospitals suspended SHA services due to unpaid claims.
Ms Isabella Lobuk, a 45-year-old mother of three had to cover her medical bills after seeking treatment for a mild respiratory infection at a private facility.
“I had to pay for my medication today. They stopped accepting SHA and I wasn’t even aware,” she said.
In Trans Nzoia County, most patients seeking outpatient services are forced to pay cash to get medical services that could otherwise have been catered by the Social Health Insurance Fund (SHIF).

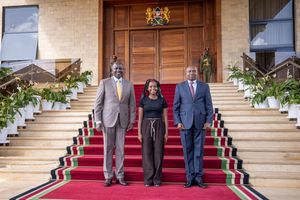
SHA Chairman Abdi Mohamed, PS Harry Kimtai and Rural Private Hospitals Association of Kenya Chairman Brian Lishenga speak to reporters on October 6, 2024.
At Crystal Medical Cottage, one of the (RUPHA) members has been affected and is not admitting patients using SHA; only those who subscribe to other medical insurance can get services.
“Last week my son was taken to Crystal Medical Cottage but he had to use Minet insurance, which is the Insurance given by my employer Teachers' Service Commission (TSC) to get services,” said Zipporah Nyongesa.
It is the same situation in neighbouring West Pokot County, where a patient Julia Chepunyorio who attends an unnamed private hospital in Kapenguria for a nerve disease and muscle atrophy was forced to pay Sh10,000 to access treatment.
“My husband was forced to sell a cow for me to get treatment," she told Nation.Africa.
Another patient Charles Kiptoo was forced to take his ten-year-old daughter with chest complications back home after he found out that private hospitals were not treating patients with the SHA medical scheme.
"My daughter used to be treated at the hospital, but now it will be hard. I don't have money to pay cash in private hospitals. She is suffering and I don't think she will get the required treatment in public hospitals, “he said.
He expressed his frustration, saying he has no means to support his daughter’s medical needs.
“We are poor, and without this insurance working, I cannot afford private hospital charges. I am appealing to well-wishers to step in and help us. My daughter is suffering, and there’s little we can do,” he said.
He said that SHA was introduced to improve healthcare access, particularly for vulnerable groups, and its ineffectiveness in covering private health facilities has left many stranded, especially those who require specialised care unavailable in public hospitals.
At Nanyuki Cottage Hospital in Laikipia County, patients who have been seeking medical services at the facility said SHA was not being accepted.
“I went there last week but was told SHIF would not be accepted. I had to pay cash to get the treatment,” said a woman who only gave her name as Joyce.
In Meru, the majority of level three and level four private hospitals we inquired from said they stopped admitting patients through the SHIF on Monday.
In Kirinyaga, a worker at a private hospital in Kerugoya town who declined to be quoted said they were not accenting SHA patients.
“There is no way we can continue treating patients while we’re not paid,” the worker told Nation.
The AGC Tenwek Hospital in Bomet has for the last one month locked out police officers and teachers from accessing medical services due to unpaid Sh215 million by Medical Administrators Kenya Limited (MAKL).

The Cardiothoracic Centre at AGC Tenwek Hospital in Bomet County on October 14, 2024.
Thousands of beneficiaries and their family members covered under the government medical cover have been turned away and can only be treated when they pay cash.
"It is unfortunate that I have been asked to pay Sh78,000 for treatment of my son who has been admitted for a week, due to the suspicion of medical cover by AGC Tenwek" ms Beatrice Bett, a teacher said.
Ms Bett said in an ideal situation, she would have only paid less than Sh500 for the treatment of her son at the hospital.
Hundreds of police officers have not accessed services at the hospital, but could not speak on record for fear of reprisal from their bosses.
The management of AGC Tenwek Hospital, in a memo dated January 29, 2025, informed stakeholders that effective 1st February 2025, the hospital will no longer provide services to members under Medical Administrator Kenya Limited (MAKL) – affecting teachers and police officers.
Dr Robert Langat, the board chairman at Tenwek Hospital confirmed that the services had been suspended due to nonpayment by the government.
"It is the board's decision that the services will only be reinstated once the payments have been made by the government for the teachers' and police officers' medical cover," Dr Langat said.
He revealed that apart from the Sh215 million owed by SHA, the defunct NHIF has not paid Sh560 million pending bills.
Dr Langat said "This was a very difficult position to take, but it had to be done to avoid collapse in hospital operations," Dr Langat said.
In Hola, Tana River County, the county's private hospitals, which once offered essential services through the government-funded SHIF card.
The hospitals argue that the government's failure to clear outstanding debts has placed a heavy financial strain on their operations, making it unsustainable to continue offering services under the SHIF framework.
"They owe us millions of money and if we continue like this, we will not have a facility here, therefore we must draw the line somewhere," said a hospital manager on anonymity.
As a result, the local population, largely reliant on the scheme due to financial constraints, finds themselves unable to afford medical care.
Many patients, especially those with chronic conditions or urgent health needs, are now forced to either seek care from distant government hospitals, which are often overcrowded and under-resourced or endure untreated illnesses.
"Currently there are no reagents to test malaria or even do a urine test in our county referral hospital, this is the third week running, and I’m forced to do tests in private hospitals which doesn't come cheap," said Halima Rashid.
"The bill that comes with consultation only can shock you, before you get to seeing a doctor and finally drugs, your condition may even worsen, and you can imagine in this one, there is no menu where you can decide whether to proceed or stop," said Ms Rashid, a resident.
However, at Kendu Adventist Hospital in Rachuonyo North, Chief Executive Officer Philip Ghai said they are yet to receive official communication from the association.

Kendu Adventist Hospital in Rachuonyo North.
"We are still using SHIF and patients admitted at our hospital are using the medical scheme to offset their bills. Information about the suspension was only in the media," he said on phone.
In Homa Bay County as well, some patients are still using SHIF cards to pay for medical bills in certain hospitals.
In Siaya, a spot check by Nation.Africa established that even though SHIF has been suspended by some private facilities, a handful still offered cardholders services albeit limited.
Mr John Owino 64, a retired teacher is a worried man after the hospital he regularly visits to monitor his health blacklisted SHIF.
“Last week I went for a check-up at a private hospital and used the SHIF without a problem. I resorted to private facilities since most of the public hospitals seldom have the drugs that I require for my medical condition,” he lamented.
“I already picked my medication for this month and part of next month. I hope by next month, the government shall have resolved the matter with the private facilities,” he added.