Is your county health chief ready for the challenge?

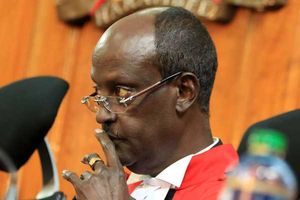
Kisumu County Acting Minister of Health Dr. Gregory Ganda during an interview with Nation journalists at his office on July 20, 2022.
What you need to know:
- Most counties struggling with health service delivery are failing at making policies
- Many national-level policy documents remain ignored at county level
- Health CECs should be innovative in coming up with ways of financing their departments
It has been a whirlwind of an election period and the dust is slowly settling. Our Senate and National Assembly representatives have been sworn in and speakers elected. The President has nominated his Cabinet and we await the parliamentary vetting process.
The same process is replicated across the 47 counties, with the county assemblies being sworn in and the speakers taking office. Many counties have newly elected governors, carrying with them the hope of improved service delivery in their regions. As governors settle into office, they must also quickly appoint their local cabinets to execute business.
It is quite a circus, with some county bosses nominating their preferred members while others advertise the posts, calling for all qualified persons to apply for the job. The lists of those lined up for the posts have started popping up on various social media platforms as they await vetting by their county assemblies.
With healthcare being largely devolved, the onus of service delivery remains a key responsibility of county governments. The health of a county heavily depends on the county executive committee member (CEC) heading the Health department. Who has your county boss nominated for this important docket?
A few counties have had the privilege of having one governor for the past 10 years.
The consistency makes it easy to evaluate their performance in the county and see how they have scored. Other counties have had frequent replacements, making it difficult to assess their impact at a personal level.
Monitoring and evaluation
As new health chiefs in the counties line up to take office, what should the people they serve expect?
The person coming in to head the docket drives the health docket to ensure that the county puts in place policies for effective service delivery, mobilises resources for the same and ensures that appropriate monitoring and evaluation systems are in place to ensure the department is headed in the right direction.
This is executed through an able team comprising the chief officer, the county director for health and the county health management team.
Most counties struggling with health service delivery are failing at the first step: policy. A good number of county health chiefs are unaware of the existing national policies with regard to various aspects of healthcare that require domestication at local level, to guide effective service delivery. Further, they may fail to appreciate the need to push for county legislation to support the same.
The laws and policies give direction on how the services should be delivered, giving rise to the implementation strategies and robust evaluation mechanisms to ensure the department remains on course.
So why, pray tell, do many national-level policy documents remain ignored at county level? First, many of these policies are developed without adequate input from the county teams, who are the ultimate implementers. The counties are brought in at the tail-end as stakeholders, instead of being part of the core technical working groups from the beginning. This lack of meaningful engagement in the process leads to lack of ownership of the final policy, hence implementation is hampered.
Gaps
In addition, there is inadequate dissemination of these documents to the end users. The development of many of these policy documents is, unfortunately, still heavily donor-funded. These budgets rarely take into account the appropriate and consistent dissemination down to the implementer for the true value of the document to be seen.
Further, the lack of appropriate induction of the county health chiefs to these documents cannot be overlooked. Many county health chiefs are not necessarily from a health background, hence require a lot of dedication to reviewing the tonnes of documents in the sector for effective leadership.
This helps reveal the gaps that arise due to the uniqueness of the county, resulting in development of targeted county laws that address them.
County health financing continues to be a challenge as the effects of ranking Kenya as a middle-income country now kick in. Health has perennially heavily depended on donor funding to run programmes. With progressive withdrawal of funding for most of these programmes, the counties are now forced to step in and take over.
Appreciating the amount of debt Kenya is in as a country, we do not expect the exchequer to perform miracles as we go along. County health chiefs have to be a lot more innovative in coming up with ways to finance their departments, especially keeping in mind that this is a sector that does not raise income.
It is time to ensure that every county facility, down to the Level Twos, are NHIF-accredited to provide the entire retinue of services as per their capacities. Further, they must push for their constituents to be NHIF contributors by all means and that money paid out by NHIF for services rendered is ring-fenced and ploughed back into the facilities.
It is time to cut back on wastage within the system, and ensure proper priority settings, to enable the shilling put into healthcare to stretch as far as possible.
The health departments should truly embrace zero tolerance to corruption because it directly contributes to preventable deaths.
The appetite for constructing buildings which remain unequipped and unstaffed, to line people’s pockets with tenders, should be curbed.
May the next five years bring to fruition what was envisaged in devolution of health.
Dr Bosire is an obstetrician/gynaecologist