Mental health recovery: How three Kenyans overcame years of misdiagnosis

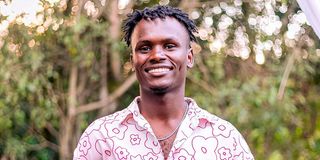
From left: Samuel Boiyo, Kelvin Ochieng and Robert Omondi. The three are rewriting the narrative by courageously sharing their mental health stories, proving that real strength lies in speaking up.
What you need to know:
- Three Kenyans share their personal struggles with mental health challenges, revealing how misdiagnosis, stigma, and financial barriers continue to plague the country's healthcare system.
- Despite challenges including high treatment costs and limited access to services, mental health experts are optimistic that policy reforms and healthcare changes could improve access to mental health care.
Picture this: You're sitting in Kibera Law Court when a young man bursts through the doors, singing at the top of his lungs, shouting incoherently, completely lost to the world around him. Your first instinct? He's dangerous. Unhinged. Someone to avoid.
But what if that moment of apparent madness was actually the beginning of salvation?
For Samuel Boiyo, that chaotic courtroom scene became his unlikely gateway to proper mental health diagnosis after a decade of suffering in silence. His story, woven together with those of two other remarkable Kenyans, reveals the complex reality of mental health in our country—where stigma and misdiagnosis continue to challenge thousands, yet where hope persists through community advocacy and sheer human resilience.
Ten-year misdiagnosis
Samuel Boiyo, now 40, can pinpoint exactly when his life took an unexpected turn. It started innocuously enough—stomach aches and headaches during high school that everyone dismissed as typical teenage complaints.
His teachers wrote off his frequent absences as laziness. His parents, watching their son's sudden mood swings and erratic behaviour, assumed he was simply being rebellious. The truth was far more complex: Samuel was battling bipolar disorder, and no one saw it coming.
For 10 agonising years, his condition was mistaken for mere physical ailments—a misdiagnosis that nearly cost him his freedom and livelihood.
"When I was 18, there was a day that I became uncontrollable, and that's when my parents noticed it was very serious," Samuel recalls. "Unlike before, when they would take me to the nearest dispensary for stomach aches and headaches, this time I was rushed to a referral hospital."
Even then, his condition continued to be misdiagnosed. Every visit to a health facility became a deeply frustrating and painful experience—repeated misdiagnoses, worsening health, and the crushing burden of stigma.

Samuel Boiyo Ngigi, a bipolar survivor and a male mental health advocate, speaks during an interview at Nation Centre, Nairobi on June 11, 2025.
The situation in his Molo village in Nakuru became unbearable. Facing severe stigma, Samuel was forced to relocate to Nairobi, only to encounter more hostility. His crisis reached its peak when residents mistook his mental health symptoms for criminal behaviour and wrongfully accused him of attempted theft at a local church.
He was arrested and arraigned in Kibera Law Court—the very place that would, unexpectedly, become his pathway to proper mental healthcare.
When the judge ordered a psychiatric evaluation at Mathari National Teaching and Referral Hospital, Samuel was finally diagnosed with bipolar mood disorder, anxiety and depression.
"I entered the courtroom singing and shouting, completely unaware of my surroundings. That's how sick I was," Samuel explains. "Those were classic symptoms, but no one recognised them until a judge ordered my evaluation. I then started my proper treatment after the diagnosis."
Road to recovery
For three crucial months at Mathari Hospital's forensic unit, Samuel underwent intensive treatment that finally brought him back from the brink. The facility scheduled sessions with psychological counsellors, psychiatrists, therapists and nurses who supported his treatment journey. His family negotiated with the person who had sued him, the case was withdrawn, and he was declared a free man in 2004.
But freedom didn't mean the end of his struggles. Samuel's life remains a rollercoaster of resilience and relapse—a stark reminder that mental health recovery is an ongoing journey, not a one-time cure.
"I have had several incidents where I have relapsed and found myself readmitted at Mathari Hospital, but sometimes I get very resilient and go to my job of hawking watches, necklaces and earrings," he says. "But during manic episodes, I lose my hawking and hard-earned money."
Financial constraints directly fuel his relapses and hospital readmissions. The death of his father during Covid-19 was particularly challenging, triggering a significant relapse.
Yet there's hope in Samuel's story. He hasn't relapsed for four years running, despite medication side effects and past trauma, thanks to strict adherence to his treatment. Changing his lifestyle and accepting his condition has helped him live more positively.
"I still have family days with a psychologist at Mathari, where we discuss why I need to take medicines for my sanity," he tells Healthy Nation.
When his father—his strongest support system—died, Samuel found new community with Survivors and Users of Psychiatrist Services. Alongside others who've faced similar struggles, they meet to share their lived experiences.
"Since I started creating awareness about mental illness, my mental health has improved drastically. When I have something disturbing me, I look for a person I can speak to, and I don't mind speaking out because I want to stop the stigma," he says.
Samuel's medication regimen—Encorate Chrono (mood stabiliser), Venlafaxine (antidepressant), and Aripiprazole (antipsychotic)—is his lifeline. But the drugs have made him live from hand to mouth.
"I spend Sh10,000 monthly on my medication," he reveals.
He urges the government to create a dedicated budget for mental health during every financial year and make mental health treatment free in all government facilities like Mathari. Samuel believes that without his condition, he would have completed high school and pursued university studies to become a lawyer. He now hopes for sponsorship to study a Business Management course, acquire entrepreneurial skills, and live better while continuing his treatment.
"Mental illness is not like malaria, which requires a short course of medication. Mental illness requires long-term medication," says the father of two, noting that he has taken drugs for 20 years non-stop. "I now need support to help me go on with my medication."
Art as advocacy
Across Nairobi, we meet Robert Omondi, 28, a creative writer whose poetry has become his weapon against mental health stigma. For eight years, Robert has built his name in the mental wellness space, finding healing through advocacy.
His passion was ignited after losing two close friends—an experience that left him devastated. The diagnosis of his campus roommate with schizophrenia, and witnessing the stigma his friend faced, cemented his commitment to the cause.
The memory still haunts him: "Your friend has been seen walking naked," came the devastating phone call during examination period. Robert had no idea where to find help. He took his friend to a general hospital, where mental healthcare was an afterthought. The experience left him angry and heartbroken. His roommate later died.

Robert Omondi, a spoken word artist who uses poems to educate men on mental health. In 2022, he won the World Mental Health Day Poetry Writing Competition by Kenya National Commission on Human Rights.
In 2019, shortly after former President Uhuru Kenyatta declared mental health a national concern, Robert and his friends organised a walk on World Mental Health Day that attracted about 2,000 participants. They then formed Youth for Mental Health Consortium, an umbrella body of different young people and a peer support network.
"I once again lost a member in our arts group through suicide, and it was such a shock—we did not see it coming," he tells Healthy Nation. "It took a while to bounce back from it, and I remember the only thing that helped us translate the grief and come to terms with it was writing poetry pieces that captured that moment."
Robert believes there is no health without mental health, and he sees a strong connection between art and mental health advocacy. Having consistently sought support through sessions with psychologists or psychiatrists, he pursued a Diploma course in Quality Rights in Mental Health offered by the World Health Organisation, integrating this knowledge with his artistic writings.
A poem he wrote and performed during the 2021 World Mental Health Day Poetry Writing Competition won him an Outstanding Performance award hosted by the Kenya National Commission on Human Rights.
"The poem condemns societal cultures and stereotypes on mental health that lead to people being tied using ropes or chains. It also appreciates caregivers who help patients seek medical services," says Robert. "I tell people through poetry that harassing someone based on their condition is a violation of human rights."
According to 2024 statistics by the Ministry of Health's District Health Information System, Nairobi County recorded 53,521 cases of mental disorders—a staggering figure that underscores the magnitude of the challenge.
In light of these numbers, Kelvin Ochieng, a 21-year-old certified mental health trainer, emphasises the importance of advocacy among teenagers within Nairobi's informal settlements. He believes this approach will significantly reduce mental health cases among young people in these vulnerable communities.
"After one of us was taken to a hospital, diagnosed, and found to be depressed—but he didn't know—that's when we started describing what mental health wellness is," Kelvin explains. "We then moved on to how someone can find themselves in that space of being mentally unhealthy and, crucially, how you can come out of that space."
Kelvin Ochieng is a youth who organises church ministries on mental health for young people within Nairobi's informal settlements.
Born in Nairobi's Mukuru kwa Njenga informal settlement, Kelvin says living almost half his life in the area exposed him to the struggles that trigger mental illness. His environment changed when he received a scholarship to pursue Theology and Psychology in Uganda, but the memories of mental health struggles he witnessed remain vivid, fuelling his dedication to advocacy.
"Growing up in a slum is not easy. It has its share of mental health triggers like insecurities, drugs and substance abuse. Lots of my friends were killed with gunshots," he states. His experiences extended to personal brushes with the law: "I have gone to the cells several times, not because of my problems but because of the companies that I kept, so I have seen these things."
Kelvin leads a group of approximately 80 teenagers drawn from various churches within Nairobi's informal settlements, facilitating monthly sessions focused on mental health wellness.
"I ask questions to trigger teenagers, and then they respond because they are informed. The moment you make teens not participate or speak from their hearts, they tend to sieve information, but when you allow them to speak, you'll realise how much they know. So mine is to offer guidance," Kelvin explains.
He uses his knowledge from theology, psychology and mental health training to connect mental healthcare and spirituality, inviting hospital experts during sessions to provide science-based mental health talks.
"When you are stable mentally, it means you are able to function. The things we see, interact with, listen to, and process greatly make our mental health deflate," says Kelvin. "It is good to make sure that our lives revolve around building our minds, not deflecting them, yet most teenagers are not able to sieve good things for their mental health."
As a professional DJ, Kelvin finds his own mental nourishment through music. "Anytime I play music for people, I want them to be part of it and live in that moment. I am very careful about what I feed people behind the wheels because whatever you feed your mind, out of the abundance of the heart come issues of life."
During the launch of the Nairobi City Mental Health Strategic Action Plan, Stella Waruingi, a mental health expert who leads mental and psychosocial support services for Nairobi County, explained that the policy document offers a five-year roadmap for mental health matters.
"If we pick from this document, we are talking about promotion of mental health, leaving no one behind, and in this promotion, we have gone further and anchored it at the community level, where most of the work is taking place. That is where we want to address it, forming safe spaces," she says.
Stella notes that young people like Kelvin and Robert, who are holding conversations that promote mental wellbeing at the community level, align well with the action plan's highlights.
"Next is screening for preventive mental wellbeing for those who are at risk, and we know our population is very much at risk of mental health. Look at the issues we have of gambling, the political landscape is not favourable for the community, unemployment, drugs and substance abuse, gender-based violence, and lack of basic access to water and sanitation," Stella adds.
Despite having mental health specialists in the country, Stella says there's need to integrate mental health into primary healthcare and create comfortable rooms for individuals to seek mental health services.
"The stigma associated with mental illnesses prevents individuals from seeking help. You know people think mental illness is only for people in Mathari, but we want to break that stigma and take these services where you go," she explains.
While individuals like Samuel continue to face the high cost of daily mental health treatments and medications, Stella remains hopeful that financial hurdles preventing Nairobi County's health facilities from offering these crucial services will soon be overcome.
"I am very optimistic that if SHA works the way it is supposed to, where a health facility has the money—because the problem is the money—then it is going to be a game changer for access to mental health services," she concludes.





