Kenya beats global TB targets, but aid cuts threaten to erase progress
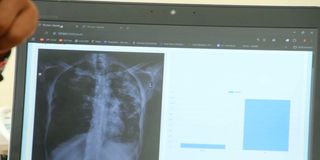
A chest radiograph being investigated for TB using an AI tool at Karatina Level IV Hospital in Nyeri.
What you need to know:
- These results reflect Kenya's high case detection rate, which now exceeds 80 per cent, placing the country among the most successful globally in identifying TB cases.
In a significant public health achievement, Kenya is among the only 49 countries worldwide that have met the first-phase targets of End TB Strategy, as set out by the World Health Organization (WHO).
In its newly released Global TB 2025 Report, WHO notes that Kenya has successfully reduced the incidence of tuberculosis by at least 20 per cent and tuberculosis-related deaths by 35 per cent between 2020 and 2024, positioning it as a leader among African nations in the fight against the deadly disease.
Despite remaining on the WHO's list of 30 countries with a high TB burden and being classified as a country with a high TB/HIV burden, the report shows that between 2015 and 2024, Kenya exceeded its initial targets by reducing the incidence of the disease by 20 per cent and the mortality rate by more than 50 per cent.
The country now falls into the endemic category, with a rate of 100 to 299 cases per 100,000 people in 2024.
"Several high TB burden countries in the WHO African region have achieved reductions of 50 per cent or more (such as Kenya, Nigeria, Uganda, Tanzania and Zambia)," reads the report.
These results reflect Kenya's high case detection rate, which now exceeds 80 per cent, placing the country among the most successful globally in identifying TB cases.
Similarly, more than 90 per cent of TB patients now know their HIV status, making Kenya one of 32 African countries to have achieved this critical milestone, and demonstrating the successful integration of care systems.
For instance, the National Tuberculosis, Leprosy and Lung Disease Programme has transformed the country's response to TB by expanding diagnostic capacity through the use of rapid molecular testing and community-based screening, which has been effective in targeting high-risk populations and rural communities.
Kenya has also made notable advances in TB preventive treatment, especially for household contacts and people living with HIV, aligning with the WHO's ambitious goal of achieving 90 per cent preventive therapy coverage by 2027.
The country has equally established robust data and surveillance systems, completing multiple assessments, including a TB prevalence survey in 2015, a national inventory study in 2013, and continuous drug resistance surveillance since 2020.
However, these achievements are now facing a hurdle in the form of cuts to international funding. The Global Fund has cut its allocations by Sh180.9 billion ($1.4 billion) for 2025, which is an 11 per cent reduction, while the US Agency for International Development (USAID) has scaled back its bilateral support to 24 priority countries, including Kenya.
Domestic funding
USAID funding accounts for 10 per cent to 20 per cent of the budget for Kenya's National TB Programme, while these donors collectively provide 40 per cent to 50 per cent of its financing.
While the government has increased domestic funding in response, substantial gaps remain. WHO has placed Kenya among 17 countries requiring close monitoring for potential service disruptions.
Despite the success, significant structural challenges persist. According to national survey data, nearly half of TB-affected households face catastrophic health costs exceeding 20 per cent of household income. Undernutrition, HIV and poverty continue to fuel transmission.
Kenya's Universal Health Coverage Service Coverage Index was approximately 55 out of 100 in 2021, which is above the African average of 44 but below the global average of 68. This leaves many patients without adequate social protection.
Regionally, Africa reduced TB incidence by 28 per cent and deaths by 46 per cent between 2015 and 2024, outperforming all other WHO regions and exceeding the first End TB
Strategy milestones.
Similarly, the region has shown sustained year-on-year reductions in TB deaths since 2011, representing the best regional performance globally.
Kenya has now joined Nigeria, Uganda, Tanzania and Zambia in achieving a mortality reduction of at least 50 per cent. The African region currently accounts for 25 per cent of the global TB burden.
Globally, the incidence of TB has fallen by just 12 per cent since 2015, and deaths have fallen by 29 per cent. These figures are far below the 2025 milestone targets of reducing both by 50 per cent.
According to WHO, the world is severely off track to meet the 2025 milestones or the 2030 targets of reducing the incidence by 80 per cent and the mortality by 90 per cent.
In 2024 alone, an estimated 10.7 million people developed TB worldwide, with an incidence rate of 131 per 100,000 people, and 1.23 million people died from the disease, including 150,000 people living with HIV.
The case fatality rate is 11.5 per cent. Although 2024 saw the first decline in cases since 2020, with incidence levels returning to those seen in 2020 after consecutive increases from 2021 to 2023, progress is still too slow.
Drug-resistant TB is also becoming a serious issue, with 390,000 new cases of multidrug-resistant or rifampicin-resistant TB in 2024. However, only 164,545 people were enrolled in treatment, representing just 42 per cent coverage.
Despite this burden, the global TB response is facing a significant funding shortfall. In 2024, only Sh762.5 billion ($5.9 billion) was available, compared to an annual target of Sh2.8 trillion ($22 billion) by 2027, creating a Sh2.1 trillion ($16.1 billion) funding gap.
"Funding for the TB response remains grossly inadequate and has been stagnating. Funding for the provision of TB prevention, diagnosis and treatment amounted to $5.9 billion in 2024, and funding for TB research was $1.2 billion in 2023. These figures are 27 per cent and 24 per cent respectively, of the global targets of $22 billion and $5 billion annually by 2027," reads the report.
It is projected that this funding cut could lead to an additional 500,000 to two million deaths and 1.4 to 10 million additional cases globally, threatening to reverse years of progress.





