Faith Ohana holding her baby outside her house in Kibra, Nairobi and Josephine Awino who lost her baby after being turned away by healthcare worker.
A teary Josephine Awino recalls the night she gave birth on the road. She had staggered from her house with her husband’s help, trying to reach the hospital. As they navigated the narrow alleys of Kibra, surrounded by tin-roofed houses, her pain intensified. Earlier that night, she had hoped the healthcare workers were right – that her pain was not related to labour and would subside. But they were wrong.
“I first felt the pain around 1am. I went to the hospital, but the clinician in charge dismissed me, so I walked back home,” she tells Sunday Nation.
At home, the pain escalated, cutting through her body. She gritted her teeth through it until she realised it wasn’t going away. It didn’t.
It was a familiar pain, and Josephine knew her baby would come at any moment. Her husband escorted her to a local health centre, where she had been attending antenatal clinics.
“When I arrived, the clinician in charge told me to go home, that I wasn’t ready to deliver that night. I didn’t want to go home, but I had to listen. I was in so much pain, yet they weren’t ready to help me,” she recalls.
Josephine says that no test was performed to confirm she wasn’t in labour. The decision was based on the clinician’s instinct, not clinical assessment. She went home regardless.

Josephine Awino, who lost her baby after being turned away by healthcare worker. She later gave birth on the road.
“I knew I was in labour because it wasn’t my first time. I told my husband we needed to go back to the hospital. He knows I rarely complain, even when I need help, so he understood how serious it was,” she says.
He agreed to accompany her back to the same facility that had turned her away earlier.
A few metres from their home, her water broke. Few people were on the road, mostly matatu operators who had no experience with childbirth. Her husband was frantic, pacing back and forth, hoping for help.
When it became clear no one would come, she pushed, and the baby was born—silent, covered in blood.
Matatu operators helped get her to the hospital.
“When I arrived, the clinicians who had dismissed me told me not to tell the doctor on duty that I gave birth on the road. They coached me on what to say, telling me to claim my baby died in the hospital. That still disturbs me,” she says.
“My baby lay lifeless, tagged with my name. Every time I remember that, it pains me. I feel like I left a part of me in the hospital. She could have been my second daughter,” Josephine adds.
She believes her child could have been saved if the healthcare worker had listened to her.
“I wish all clinicians had empathy,” she says.
A few blocks from Josephine’s home, 25-year-old Faith Ohana cradles her baby. It’s cold outside, and the grey clouds are thickening. She is alone in the house with her seven-month-old, who smiles when we enter.

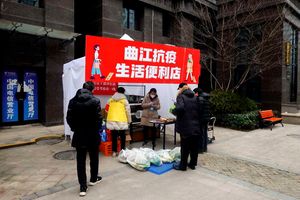
Faith Ohana holding her baby outside her house in Kibra, Nairobi, on May 9, 2025.
Last year, in this very house, her water broke when she was alone. Neighbours heard her moaning and came to her aid. She gave birth at home with unskilled assistance.
This is her first child.
When Faith visited the hospital for antenatal care, she was asked to have a scan, but she didn’t have the money.
“They asked for Sh2,500. I didn’t have it. They told me if I didn’t get the scan, I shouldn’t return to their facility. So, I opted to give birth at home,” she says.
“Giving birth at home was one of the worst decisions I made. I have endless backaches, and I can’t afford to go to the hospital for treatment. My baby is fine, but my health hasn’t been the same since I gave birth,” she adds.
Faith went to a public hospital but feared she’d be turned away for not having a scan. She had no one to guide her and no money.
“I had registered for the Social Health Authority, but it doesn’t cover scans. I also registered for Linda Mama, but it no longer works. I wish the government would include such services under SHA for women like us who can’t afford out-of-pocket costs,” she says.
Recent data from the Kenya National Bureau of Statistics’ Economic Survey shows fewer women gave birth in hospitals in 2024. The number of deliveries at health facilities decreased by about 3.2 per cent compared to the previous year.
This decrease is seen across all modes of delivery except caesarean sections, which saw a slight increase of 0.6 per cent, totalling 220,505 deliveries in 2024. Vaginal births, however, dropped to 2020 levels, which corresponded with the lockdown period during the pandemic.
Assisted vaginal deliveries also decreased from 4,729 in 2023 to approximately 3,902 last year.
A 2020 study published in the East African Health Research Journal explains that home births, particularly unassisted ones, can result in excessive bleeding and complications like retained placenta.
The neonatal mortality rate for unassisted home births is double that of hospital births. Babies born in such conditions are at higher risk of complications such as oxygen deficiency, infections, respiratory distress, hypothermia, and prematurity.